 Hepatitis A:
Hepatitis A:
HAV infection occurs throughout the world but is most prevalent in developing countries. Approximately 1.5 millions clinical cases reported worldwide annually, a figure that greatly underestimates the true incidence of infection.
(Nelson Text book of Pediatrics Vol 2 1680 and Hepatology 43(2) S1 2006)
HAV is transmitted commonly most via fecal oral route. Its prevalence is high in regions with low standards of sanitizations. HAV virus is stable at ambient temperature and at low pH. Most of this virus appears to be produced in liver and to reach intestinal contents by secretion from infected hepatocytes via the biliary system. Fecal shedding of the virus reaches its maximum just before the onset of hepatocellular injury at which point the most infectious. The mechanism responsible for hepatocellular injury in hepatitis A is poorly understood. Clinical Chemistry 43:8(B) 1494–1499 (1997)
Hepatitis B (HBV):
Liver disease due to HBV is an enormous problem globally. Unlike HAV, HBV remains in the blood during the last stages of a prolonged incubation period (4 to 26 weeks) and during active episodes of acute and chronic hepatitis. Infection with HBV is defined by the presence of HBsAg. HBV, the cause of serum hepatitis can produce
(1) Acute hepatitis
(2) Non-progressive chronic hepatitis
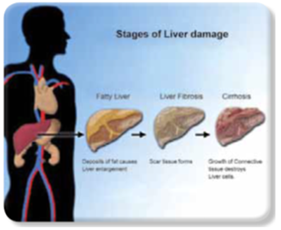
Shared blood and body fluids are the primary means of transmission. Spread from one person to another person in I.V. drug users, needle stick accidents among health workers and homosexual activities. Patients infected with HBV have different disease stages, which accompanies with varying degrees of liver damage. The incubation period of HBV is 40-150 days, with an average of approximately 12 weeks. Inactive carriers remain infections to others through parenteral or sexual transmission. Sometimes inactive carriers may develop chronic hepatitis.
Hepatitis C (HCV):
HCV is another major cause of liver disease worldwide. It is believed to be one of the most important causes of transfusion associated hepatitis being responsible for 90 to 95% of all cases. In contrast to HBV, HCV has a high rate of progression to chronic disease or eventual cirrhosis, exceeding 50%. HCV has a viral incubation period of approximately 8 weeks. Most cases of acute HC infections are asymptomatic. A characteristic feature of HCV infection is the repeated bout of hepatic damage due to reactivation of pre-existing infection or emergence of an endogenous, newly muted strain. Cirrhosis can be present at the time of diagnosis or may develop during a period of 5-10 years. Clinically, HCV hepatitis may be milder than that of HBV, but individual cases may be severe and indistinguishable from HAV or HBV hepatitis. In chronic HCV infection, a characteristics clinical feature is episodic elevation in serum transaminases with intervening normal or near normal periods. (Robbins Pathological basis of Disease6th edition)
Hepatitis D:
HDV is unique RNA virus that is replication defective, causing infection only when it is encapsulated by HBs Ag. Thus, HDV causes hepatitis only in presence of HBV. Simultaneous co-infection with HBV and HDV results in hepatitis ranging from mild to culminant diseases more likely (about 3% to 4%) than with HBV alone. HDV RNA is detectable in the blood and liver just before and early days of acute symptomatic diseases.
Hepatitis E:
It is an Enterically transmitted, water-borne infection. In most cases, the disease is self-limited; HEV is not associated with chronic liver disease or persistent viremia. Before onset of clinical illness, HEV RNA and HEV virions can be detected in stool and liver. The onset of rising serum transaminases, clinical illness & elevated IgM anti-HEV titers are virtually simultaneous.
Hepatitis G (HGV):
HGV is similar to viruses in the Flaviviridae family, which includes HCV. HGV can be transmitted by blood transfusion. HGV co-infection is observed in 6% of chronic HBV infections and in 10% of chronic HCV infections. However, whether HGV is actually pathogenic in humans remains unclear.